How to Heal a Hamstring Strain Fast and Restore Strength
A strain can stop you quickly. Running feels uncertain, walking becomes guarded, and even sitting can bring discomfort along the back of the thigh.
What slows recovery isn’t just the injury itself. It’s not knowing when to rest, when to move, or how to progress without causing another setback.
If you’re trying to learn how to heal a hamstring strain fast, the answer isn’t pushing through pain or waiting too long to act. Recovery works best when it follows stages that protect healing tissue early and rebuild strength gradually as movement returns.
Step 1: Acute Care (Right After Injury)
Early care is about protecting the injured area and calming symptoms. This phase sets up how well movement and strength return later.
If walking causes a limp, reduce load temporarily and avoid movements that increase pain. Full rest is not needed, but pushing through symptoms can delay healing.
Use the RICE approach early:
Rest: Avoid painful activity and reduce load as needed
Ice: Apply short sessions throughout the day to manage pain and swelling
Compression: Use a sleeve or wrap for light support
Elevation: Elevate the leg when resting to reduce swelling
Avoid heat, deep massage, alcohol, and stretching into pain during this phase. As swelling decreases and walking feels easier, the body is usually ready for the next stage.
Step 2: Gentle Recovery (When Walking Improves)
This phase begins once walking feels steadier and pain stays mild. The goal is to reintroduce movement without irritating the healing tissue.
Start with short, pain-free walks on flat ground. Keep your pace relaxed and increase distance only if symptoms stay calm during and after.
Add light muscle activation to support healing. Isometric hamstring holds help wake the muscle without movement. Glute activation is just as important, since weak glutes often place extra strain on the hamstrings.
Ice can still be used after activity if the area feels tender. Gentle stretching of nearby muscles, like the front of the thigh or hips, is usually better tolerated than direct hamstring stretching at this stage. Stop if pain increases or lingers.
A simple daily rhythm helps guide progress:
Morning: Short walk and isometric holds
Midday: Glute activation
Evening: Ice if needed and note how the leg feels
This stage bridges rest and strengthening. When movement feels easier and symptoms settle quickly, the body is ready for the next phase.
Step 3: Progressive Strengthening (Key Healing Phase)
This phase rebuilds strength so the muscle can tolerate load again. The goal is control first, then a gradual increase.
Controlled loading: Exercises are slow and deliberate to rebuild strength without irritating healing tissue.
Eccentric focus: Movements that strengthen the muscle as it lengthens help improve durability and reduce re-injury risk.
Glute support: Strong glutes reduce strain on the hamstrings during sports, walking, and running.
Core stability: Better trunk control helps distribute force and limits excess stress on the leg.
Pain-guided progression: Mild effort is expected, but soreness should settle quickly and not linger into the next day.
Strength sessions are usually spaced out with rest days in between. When movement feels steady and symptoms remain calm, progression is appropriate.
A physical therapist can help adjust loading and technique as strength improves.
Step 4: Return to Activity (When Strength Returns)
This phase focuses on restoring movement without triggering a setback. Progress is guided by how the body responds, not by rushing intensity.
Return to activity is usually appropriate when:
Walking feels easy: You can walk comfortably for longer periods without fatigue or symptom flare-ups.
Strength is balanced: The injured side feels similar to the other leg during basic strength tasks.
Motion is smooth: Full movement is available without pulling, catching, or sharp pain.
Progress back into activity gradually:
Walk-jog intervals: Alternate walking and easy jogging at a conversational pace.
Controlled running: Add short, controlled strides before increasing distance or speed.
Sport-specific work: Reintroduce quick starts, stops, or changes in direction only once earlier steps feel stable.
Warming up thoroughly and continuing strength work during this phase is important. Early return is when re-injury risk is highest, so quality movement matters more than volume. When progress feels steady and symptoms stay calm, activity can continue to build safely.
Nutrition and Supportive Care During Recovery
Recovery is about more than just exercises. Physical therapy guides the process, while nutrition and daily habits help your body respond to strengthening and movement as you heal.
Physical Therapy Comes First
Physical therapy plays an important role in recovery. The steps above are best understood and applied with the guidance of a physical therapist, who can help match exercises and progression to how the tissue is healing.
The focus is on rebuilding strength, improving movement control, and helping the muscle handle load again without flare-ups. Some treatments may be used to ease pain, stiffness, or swelling, but they are supportive only.
Long-term improvement comes from gradually strengthening the muscle and returning to activity the right way, not from passive treatments alone.
Protein Intake to Support Tissue Repair
Protein helps your body repair muscle while strength is rebuilding. It works best when spread across the day instead of eaten all at once.
Include protein at each meal
Use simple foods like eggs, yogurt, chicken, fish, beans, or tofu
Add a small protein snack or shake if your activity level increases
Hydration and Daily Fuel
Drinking enough water supports circulation and can help reduce cramping as activity picks up. Eating balanced meals gives your body the energy it needs to handle rehab and gradual increases in movement.
Supportive Tools for Comfort
Some people find added comfort with kinesiology tape or compression wear during activity. These tools may help with awareness or mild swelling, but they are optional. Progress still comes from consistent strengthening and guided rehab, not from equipment alone.
How Long Does a Hamstring Strain Take to Heal?
How long a hamstring strain takes to heal depends mainly on how severe the injury is. Activity level, prior injuries, and how early the right kind of rehabilitation begins also matter.
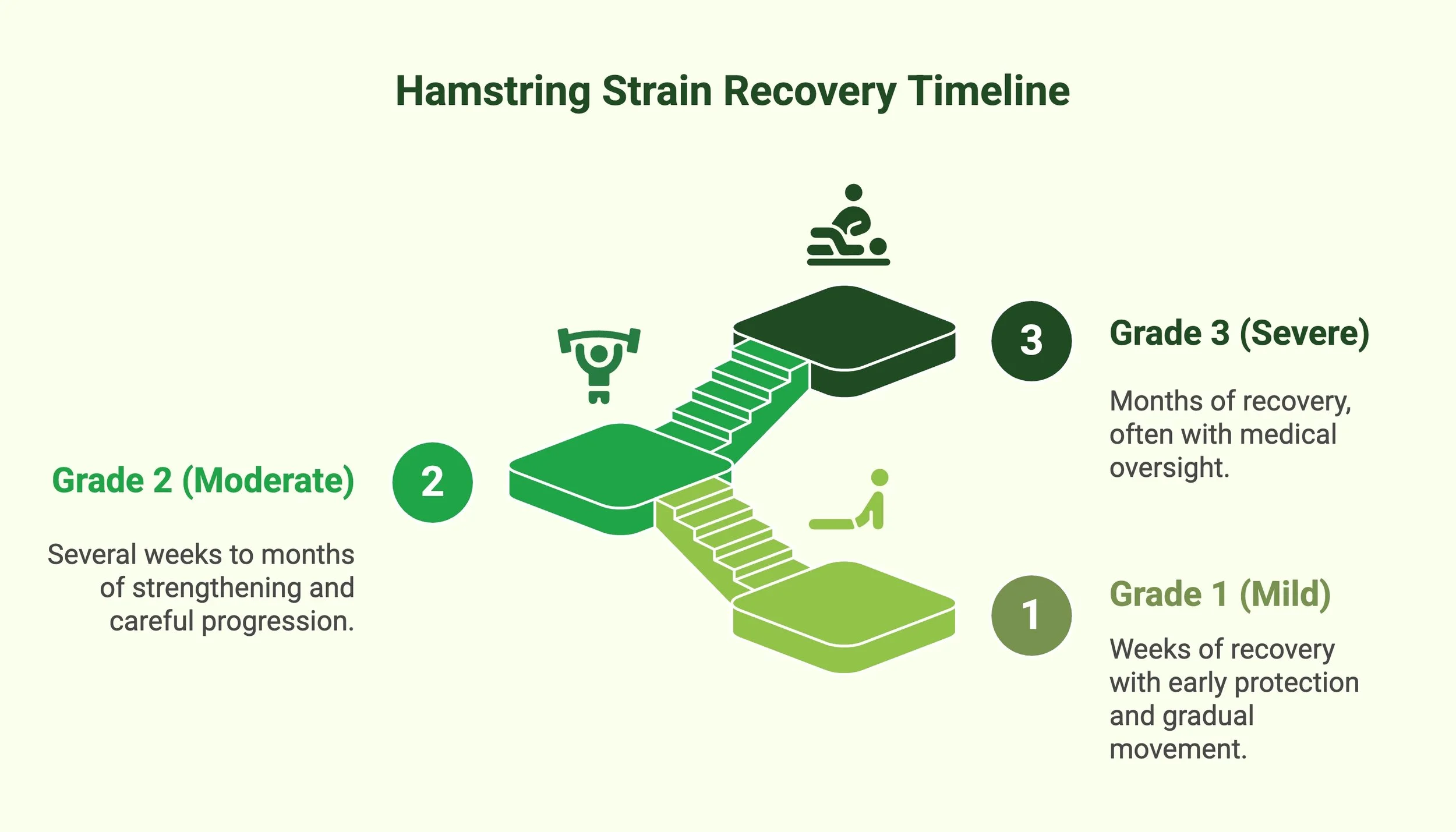
Healthcare providers group hamstring strains into three grades, ranging from mild to severe:
Grade 1 (Mild): Often improves over the course of weeks with early protection and gradual return to movement. Daily activities usually become more comfortable as pain settles and strength rebuilds.
Grade 2 (Moderate): Commonly takes several weeks to a few months. Partial tearing requires consistent strengthening and careful progression before higher-demand activity feels safe.
Grade 3 (Severe): Often requires months of recovery, especially if tendon involvement or surgery is involved. These cases need close medical or physical therapy oversight.
Even with these general grade-based expectations, recovery does not follow an exact timeline.
Moving at a pace that feels steady and controlled often leads to a smoother, safer return to activity.
Where Strength Comes Back
Learning how to heal a hamstring strain fast comes down to timing and follow-through. Protecting the injury early, restoring movement gradually, and rebuilding strength in the right order all reduce setbacks and support a safer return to activity.
Skipping steps or rushing the process often leads to repeated pain and a longer recovery. Physical therapy helps guide that progression by matching rehab to how the tissue heals, not to a fixed timeline.
If you’re unsure how to move forward or want support returning to activity with confidence, contact us today for guidance that keeps recovery on track.
Frequently Asked Questions
How do I know if my hamstring strain is serious?
A more serious strain usually causes sharp pain, swelling, bruising, or difficulty walking normally. Pain that worsens with activity, limits weight-bearing, or does not improve over time may signal a moderate or severe injury and should be evaluated by a healthcare professional.
Should I rest completely after a hamstring strain?
Complete rest is usually not needed. Early on, reducing painful activity helps protect the injury, but gentle movement supports circulation and healing. As pain settles, gradually reintroducing movement is important. Staying inactive too long can slow strength recovery and increase the risk of re-injury.
Is stretching helpful for a hamstring strain?
Stretching can be helpful later, but not right away. Early aggressive stretching may irritate healing tissue. Gentle movement and nearby muscle flexibility are usually better tolerated first. Direct hamstring stretching is typically added only after pain decreases and strength begins to return.
Why do hamstring strains keep coming back?
Repeat strains often happen when strength and control are not fully restored. Weak glutes, poor core stability, or returning to activity too soon can overload the muscle. Progressive strengthening and guided return to movement help reduce the chance of re-injury.
When should I see a physical therapist for a hamstring strain?
Seeing a physical therapist can help if pain limits activity, recovery feels stalled, or the injury keeps returning. Physical therapy helps match exercises and progression to tissue healing, improving strength and movement control while reducing setbacks during return to activity.